The Relationship Between Tobacco and Oral Health Throughout History and Culture

This article explores the origins of tobacco and its global dissemination. Historically, tobacco accompanied migrating communities, gradually spreading to various regions worldwide. Initially, its use may have been rooted in medicinal practices, with little awareness of its health risks. While much has been documented about tobacco’s detrimental effects on oral and general health, less attention has been paid to its historical contexts, such as its role in religious rituals or as a remedy for ailments.
In the 21st century, despite widespread knowledge of its harmful effects, some still perceive tobacco as beneficial—believing it aids dental health, enhances concentration, or provides a source of engagement. This article aims to renew awareness of the health risks associated with tobacco and similar products.
About Tobacco
Tobacco has long been a widely embraced substance despite its well-documented health risks. Despite widespread knowledge of its drawbacks, tobacco continues to be cultivated, refined, advertised, marketed, and sold, generating substantial economic revenue through excise duties for governments.
Numerous studies across various nations have underscored the potential harms of tobacco use on nearly every living organism’s systems, regardless of how it is consumed. Efforts to raise awareness about these effects are frequently seen in newspapers and through both print and electronic media, which paradoxically both promote and publicize tobacco and similar products while also highlighting their health hazards.
Research indicates that a significant majority of heavy drinkers are also heavy smokers, far exceeding the proportion in the general population. Additionally, smokers are statistically more likely to consume alcohol compared to non-smokers.
Understanding how and why this noxious plant’s leaves gained popularity and became addictive for humanity remains an essential part of the narrative, despite the considerable knowledge already amassed on its detrimental effects.
Historical Aspects
Throughout history, tobacco, sourced from the Nicotiana plant of the nightshade family native to the Americas, has played a significant role. Archaeological evidence traces its use back to the first century BC, where the Maya people of Central America employed tobacco leaves in sacred ceremonies. Over time, its popularity spread northward to the Mississippi Valley as migrating Maya communities shared their cultural practices with neighboring tribes.
Initially used by Native American shamans for religious purposes, tobacco also found application in traditional medicine to treat a variety of ailments such as asthma, earaches, and fevers. As European explorers like Columbus encountered it, tobacco gained global attention, with its use diversifying into pipes, cigars, and snuff, thanks in part to Portuguese and Spanish sailors who facilitated its spread worldwide.


Today, tobacco cultivation serves as a significant cash crop in many countries, contributing to government revenues through excise taxes. Major producers include China, the USA, India, Brazil, and former Soviet states. In regions like South and Southeast Asia, tobacco is integrated into cultural practices such as betel quid (paan) chewing.
The tobacco industry remains a major economic driver, supporting numerous jobs and contributing substantially to advertising, media, and government revenues, both domestically and internationally.
Various Forms of Tobacco
Tobacco is used in various forms across different countries. In South Asia, it is predominantly consumed through smoking methods such as hukka (water pipe), chilam (clay pipe), cigarettes, bidees (rolled tobacco), and Chchuta (reverse smoking). Non-smoking forms include snuff/naswar (finely powdered tobacco for inhalation), mawa, qiwam, gutkha, kheni (tobacco mixed with lime), zarda, and betel quid with tobacco. In Indonesia, tobacco mixed with clove is common and used by placing it in the oral cavity.
In central and western India, paan has gained popularity among men, whereas in Bangladesh, both educated and uneducated women are frequent consumers of paan, often with tobacco. According to a survey, Bangladeshi women who use tobacco-laced paan believe it enhances their focus on work and improves dental hygiene by strengthening teeth and eliminating bad breath.
Influences on Tobacco Use
Influences on tobacco use are complex and varied. Despite increased awareness and educational efforts aimed at discouraging smoking and alcohol consumption, both remain significant contributors to various health issues over prolonged use.
Cultural factors play a crucial role in tobacco consumption. Many individuals develop nicotine dependence influenced by familial habits; boys observing their grandfathers or fathers smoking often perceive it as a masculine trait, associated with authority and manhood. Conversely, in many societies, smoking by women is frowned upon, viewed as both morally and sexually inappropriate.
Moreover, smoking and chewing paan can be social activities that signify hospitality and strengthen friendships. In rural cultures, hookahs, clay pipes with tobacco (chilam), and shisha are commonly used in social gatherings, while some urban restaurants now cater to younger crowds with shisha clubs. Havana cigars are reserved for celebrations, symbolizing status and prestige.
Promotion and Acceptance
In India, users of gutkha argue that it helps reduce stress, aids concentration, fights bad breath, and keeps them engaged. A decade ago, cigarettes were primarily promoted through cinema and print media. However, amendments in the law now prohibit the advertising of any form of smoking tobacco in public spaces, and these messages are disseminated through print media to inform the public. Despite this, Indian cinema continues to depict male stars smoking stylishly, influencing the younger generation to emulate this behavior.
On satellite TV and the big screen, Indian cinema idols are seen endorsing various brands of gutkha, contributing to its promotion and popularity. Gutkha, marketed in colorful and appealing sachets by multiple companies in India, is perceived by youth as modern, acceptable, and fashionable, leading many to become addicted. In the UK, mothers of Asian descent blame the media in these countries for introducing gutkha to children.
This influence profoundly affects schoolchildren, as evidenced by studies reporting that many use their pocket money to buy gutkha. Some companies even promote tobacco as a dental hygiene product by including it in toothpastes or toothpowders, despite laws prohibiting such use without disclosure on packaging.
According to a survey by Chaudhury, tobacco product use among 13- to 15-year-olds ranges from 6% to 68%. In the USA, split tobacco gained popularity thanks to sports icons.
Health Risks
Health risks associated with tobacco are substantial and multifaceted. Tobacco and its smoke contain a vast array of harmful compounds, numbering over 2550 in tobacco itself and exceeding 4000 in tobacco smoke. Among these are at least 43 known carcinogens like nicotine, nitrosamines, and radioactive elements such as polonium 210.
Furthermore, tobacco smoke includes toxic substances like carbon monoxide, thiocyanate, residues of herbicides, fungicides, and pesticides, as well as tars and numerous other chemicals that can provoke diseases and compromise the body’s natural defenses. These toxic substances have detrimental effects on nearly every type of cell in the body.
Smoking primarily impacts the immune system, leading to immunosuppression and disrupting host-parasite interactions. Whether smoked, chewed, or inhaled, tobacco consumption is not only harmful but also highly addictive. Researchers have unequivocally linked tobacco use with adverse health outcomes encapsulated by the “three Ds”: death, disease, and disability.


The effects of tobacco extend across interconnected bodily systems, exacerbating health hazards and compromising various functions. Substances like tar, nicotine, and nitrosamines found in tobacco are strongly linked to oral cancer on a global scale. In developed countries, smoking is implicated in more than 85% of all male cancer deaths, with significant associations to lung cancer and other conditions like chronic obstructive pulmonary disease (COPD), which contribute to high mortality rates among individuals aged 35 to 70.
Smokeless tobacco use, prevalent in many regions, significantly raises the risk of oral cancer, accounting for a substantial portion of cancer cases worldwide. Alarmingly, tobacco use among teenagers in countries like India is on the rise, highlighting ongoing public health challenges associated with tobacco addiction and its profound health consequences.
Impact of Smoking on Oral Health and Overall Well-Being
Despite growing public awareness and educational efforts aimed at discouraging tobacco use, both cigarettes and alcohol remain significant contributors to various health issues when used excessively over the long term.
It is widely recognized that smoking significantly increases the risk of cardiovascular diseases, chronic obstructive pulmonary disease (COPD), and certain cancers. The consumption of such substances that pose health risks can adversely affect the functioning of multiple bodily systems.
Smokers often exhibit distinct changes in the coloration of mucosal surfaces due to the deposition of melanin on the basal cell layer of the mucosa. The exact relationship between smoker’s melanosis (characterized by dark-brown spots) and inflammatory changes caused by heat, smoke, and inhalation, along with the absorption of external pigments, remains unclear. Tobacco-related white keratosis patches are commonly observed in smokers. Chronic smokers may also develop nicotine stomatitis, known as smoker’s palate. Verrucous carcinoma of Ackerman, a variant of squamous cell carcinoma, is notably associated with smokeless tobacco use.
Recurrent aphthous ulcers are predominantly found in individuals who do not smoke, a well-established fact in medical research. Interestingly, cessation of smoking can sometimes trigger the onset of these ulcers, although the underlying reasons remain unclear.
Regarding the impact on the periodontium, Arno et al. conducted a study involving 1016 participants to investigate gingivitis. They discovered a significant association between tobacco use and gingivitis, even after accounting for factors such as age and oral hygiene. Similarly, Ismail et al., analyzing data from the National Health and Nutrition Examination Survey, observed that smokers tend to exhibit higher scores for periodontal debris, calculus, and oral hygiene index compared to non-smokers.
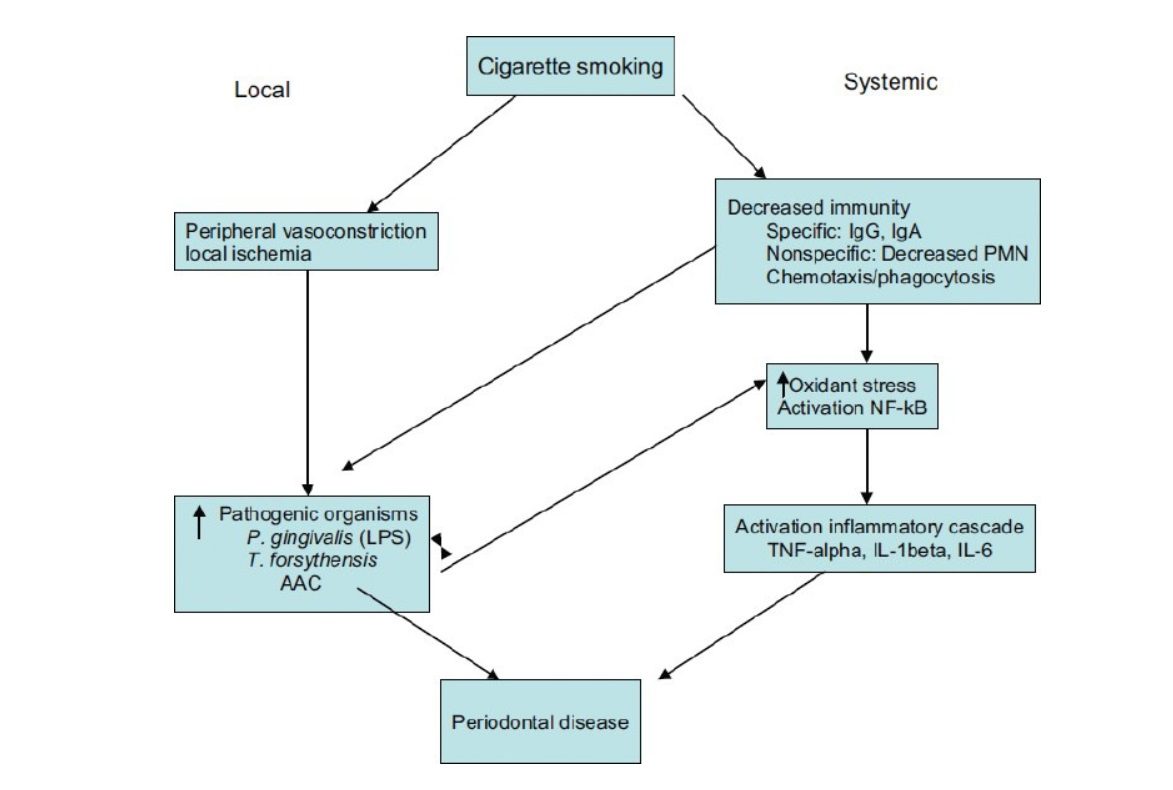
Smokers are more susceptible to periodontitis yet paradoxically less prone to gingivitis. This paradoxical behavior is thought to stem from smoking’s interference with inflammatory and immune responses, involving the activation of endothelial and inflammatory cells leading to cytokine secretion. The detrimental effects of smoking on the periodontium include changes in periodontal tissue vasculature, direct impacts on bacterial microflora, and inhibitory effects on immunoglobulin levels and antibody responses to plaque bacteria. Despite nicotine’s vasoconstrictive properties, its specific effects on gingival tissues remain challenging to quantify.
Tobacco components have been found to harm various functions of neutrophils, such as impairing chemotaxis and phagocytosis. Smokers exhibit significantly reduced motility, chemotaxis, and phagocytosis in polymorphonuclear leukocytes, weakening their ability to combat subgingival bacteria, which compromises this crucial defense mechanism. Furthermore, smoking alters antibody production, specifically affecting opsonizing IgG2 and the ratio of immune-regulatory T-cell subsets.
As a result, both innate and acquired immune responses are compromised in smokers, allowing periodontal bacteria to evade host clearance and establish themselves below the gum line. Cigarette smoking also enhances bacterial adhesion to epithelial cells and selectively promotes the growth of Gram-negative bacteria.
Changes in the subgingival environment due to smoking, including reduced oxygen levels, foster the overgrowth of anaerobic flora and opportunistic pathogens. Research indicates that smokers have significantly lower oxygen tensions in periodontal pockets compared to nonsmokers, which remains unaffected by gingival oxygen levels.
Smokers are significantly more prone to periodontal damage compared to non-smokers, with a risk increase ranging from 2.6 to 6 times higher. Tobacco smoke exposure is linked to greater susceptibility to adult periodontitis and heightened severity of the condition in smokers versus non-smokers. Numerous studies indicate that smokers typically experience more clinical attachment loss (CAL).
Research suggests that smoking as few as one cigarette per day can increase attachment loss severity by 0.5%, while smoking 10 to 20 cigarettes daily may elevate CAL by 5-10%. Higher serum levels of the nicotine byproduct cotinine have shown a direct correlation with increased CAL, deeper probing depths, and reduced alveolar crest height. Consequently, smoking significantly raises the likelihood of tooth loss by as much as 70%.
Smokers tend to have lower counts of helper T lymphocytes (Th cells), crucial for B-cell function and antibody production. This decrease results in lower levels of salivary immunoglobulin A (IgA) and serum immunoglobulin G (IgG) antibodies. Specifically, smokers exhibit diminished serum IgG2 levels and impaired IgG2 responses, potentially heightening their risk for periodontitis.
Studies have also observed reduced serum IgG antibodies against Prevotella intermedia and Fusobacterium nucleatum in smokers. Additionally, a notable 98% of acute necrotizing ulcerative gingivitis (ANUG) cases examined by Pindborg were associated with smoking. The impact of smoking on periodontal health appears multifaceted, extending beyond mere stress factors in patients. Clarke et al. demonstrated in rabbits that intra-arterial infusion of epinephrine and nicotine led to decreased gingival blood flow rates despite increased systemic perfusion pressure.
Smokers undergoing periodontal surgery using modified Widman flap or mucoperiosteal flap techniques experience significantly less reduction in pocket depth and clinical attachment gain compared to non-smokers. Heavy smoking is known to impair root coverage outcomes following free gingival graft procedures. Additionally, smokers show diminished clinical attachment gain after regenerative procedures. Miller reported a complete correlation between failure to achieve root coverage and heavy smoking (more than 10 cigarettes/day). However, heavy smokers who abstain from smoking during the initial two weeks of healing achieve results comparable to non-smokers.
Furthermore, smokers exhibit compromised healing responses following guided tissue regeneration (GTR) therapy for deep infrabony defects due to the negative impact of nicotine and carbon monoxide on wound healing.
In smokers, regenerative therapy for furcation defects has shown an 80% failure rate, possibly due to nicotine’s inhibition of fibroblast-fibronectin and collagen production, along with increased fibroblast collagenase activity.
Nicotine also suppresses the proliferation of cultured osteoblasts while enhancing osteoblast alkaline phosphatase activity. Components of tobacco can alter cytokine and inflammatory mediator production, contributing to periodontal tissue destruction.
Studies indicate that nicotine increases interleukin-6 release from cultured murine osteoblasts and elevates crevicular fluid levels of tumor necrosis factor-alpha (TNF-α) in smokers.
Smoking significantly reduces the success rates of dental implants. Smokers face a 2.6 times higher risk of implant failure between the time of implant uncovering and when the implant is loaded for restoration, particularly noted in implants for upper front teeth. Smoking also impacts healing after implant surgery and the long-term health of tissues around implants. Many clinicians consider smoking an absolute risk factor when selecting patients for implants.
In smokers, the risk of subgingival infection with Bacteroides forsythus is 2.3 times higher compared to former smokers or those who have never smoked. Smokers also show higher rates of Actinobacillus actinomycetemcomitans, Porphyromonas gingivalis, and Bacteroides forsythus. Observational studies consistently report increased plaque, calculus, and oral debris in smokers, a finding that has influenced clinical practice for nearly two decades.
Cigarette smoking is associated with elevated levels of TNF-α, neutrophil elastase activity, and prostaglandin E2 (PGE2), as well as Matrix metalloproteinase-8 (MMP8) levels in the crevicular fluid compared to non-smokers. Nicotine further enhances PGE2 and IL-1B secretion from monocytes in response to bacterial components, while increasing free oxygen radicals from neutrophils. Smokers also exhibit higher levels of metallothionein, a scavenger of free radicals, in their gingival tissue, potentially promoting a pathogenic subgingival environment.
Nicotine’s effects on IL-1 and PGE2 secretion vary depending on cell type and the presence of bacterial components, influencing the healing and regeneration potential of the periodontium in smokers.
Contemporary studies consistently show that smokers experience:
- Greater clinical attachment and alveolar bone loss
- Increased incidence of deep pockets and calculus formation
- Variable levels of plaque and inflammation
Interestingly, quitting smoking does not appear to negatively affect the response to periodontal therapy, although there are occasional reports of aphthae developing after cessation. There is a bias towards reduced signs of clinical inflammation in former smokers.

Conclusion and Comments
The link between tobacco and its various forms with numerous oral and systemic diseases, both reversible and irreversible, is widely acknowledged.
The adoption of tobacco consumption, regardless of gender, notably influences familial and cultural dynamics.
Considerable efforts have been devoted to the production, promotion, and widespread use of tobacco products. However, there is a notable lack of initiatives aimed at discouraging tobacco use by governmental and non-governmental organizations.
In many countries, health departments, trusts, and NGOs operate voluntary smoking cessation services, often integrated within hospital settings. These services typically involve counseling sessions that emphasize the potential health risks associated with tobacco use. Moreover, it’s well-documented that smoking and alcohol consumption frequently go hand in hand, supported by scientific research.
Smoking has been identified as a significant predictive factor in the outcomes of periodontal therapy. Studies on non-surgical treatments indicate that smokers experience less reduction in probing depth and fewer gains in attachment compared to non-smokers. Similarly, patients who smoke show less improvement in bone height following surgical procedures.
For implant patients, smoking is recognized as a major risk factor, impacting their overall success rates.
Furthermore, smokers exhibit delayed wound healing compared to non-smokers, as evidenced by several studies.
Additionally, research suggests that smokers tend to show poorer responses to maintenance therapy in comparison to non-smokers.